Document Functional Vision with Contrast Sensitivity and Glare
Cataract disease is a clouding of the lens which causes light scatter on the retina. This light scatter reduces image contrast and causes dimness of vision. One of the more striking problems in evaluating cataract vision loss is that many cataract patients preserve good acuity, but complain about their visual capability. The true “real-world” functional vision of cataract patients can be established as a functional acuity score using contrast sensitivity and glare testing.
Evaluation Procedure
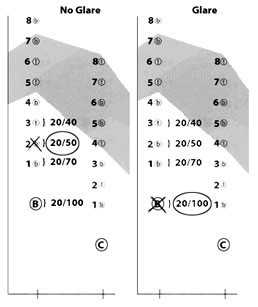
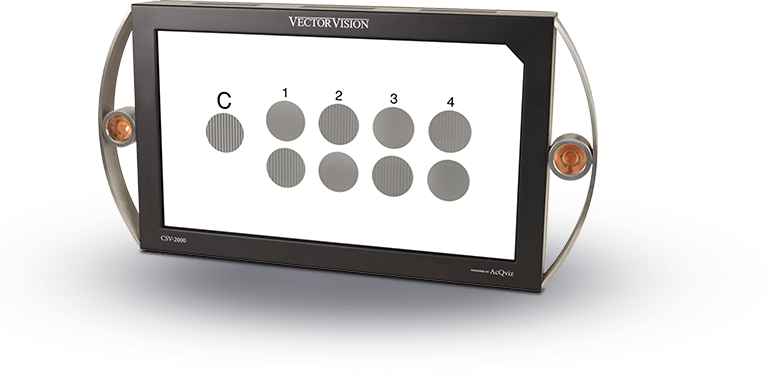
These tests are most useful for cataract patients who have good acuity, i.e. 20/40 or better. For these patients, test the patient on Row B, 6 cycles/degree, of the CSV-2000 or CSV-1000HGT and determine the lowest contrast level grating that can be identified by the patient both with and without glare. Remember that contrast sensitivity is affected by refractive error and that patients should always be tested with best correction. Determine the functional acuity from the recording chart as shown below.
The functional acuity is determined by the lowest level of contrast sensitivity that can be detected by the patient. The functional acuity score is shown in a bracket next to the contrast sensitivity score. The example shows a patient who could see the grating in contrast level 2 without glare and only the first grating with glare This patient’s functional acuity scores are circled on the example on the left. This patient has 20/50 functional acuity for contrast sensitivity and 20/100 functional acuity for glare sensitivity. These results would suggest that the patient has a significant vision problem not detected by standard acuity.
After cataract surgery, it is always best to retest the patient for contrast and glare sensitivity to demonstrate and document the tremendous improvement in functional vision. This retest is most important in patients who have normal acuity before surgery, 20/25 or better, because these patients may experience minimal or no improvement in visual acuity after cataract surgery.